I wish it were better. But the lung tumors are increasing in size. The nodes in my neck are decreasing some. But that doesn't put me at where I was in December because the tumor in the mediastinum is 1/4 inch larger, which is significant. I should get the ct scan reads shortly and I will have more detail to provide but right now I'm in a bit of a shock.
The new Dr. that I met with today recommended continuing on the Tarceva for two more months to give it a bit more time to see if it is truly played out for me. And given the major rashes on my legs, my back and my face, I would say the Tarceva is doing bloody well in other respects. If there's no change or the tumors have continued growing by the end of June, we abandon the Tarcevaand move on to radiation.
Even radiation would not be considered curative. There is no hope for that at this point. All we can hope for is to keep the cancer in check a while longer. My friend, Diane, who showed up with me, asked the Dr. towards the end of the meeting if there was anything I could do in terms of change of diet, more exercise and his response was, "Just have fun. That sort of tells me where I am right now.
Wednesday, April 28, 2010
Hat Cat
This is me 33 years ago with my cat, Dorothy Parker, outside my apartment in Lexington, KY.
My friend, Dave Cronen, who I visited in KY last week, mentioned that he was getting through a pile of old photo stuff, and might just uncover this negative. I thought I would give him a big hint as to what my print looks like these days. The years have not been exactly kind, to the print or to myself. My daughter is presently just about the same age that I am in this picture. The next year, when I turned 25, Dave gave me a blue t-shirt that had my initials on the front in yellow, and in the back it read (also in yellow), "1/4 Century." I was slightly offended at the time, but now it's a great memory. Just like most of the memories associated with Dave, from stoop sitting, to watching the Godfather on the Sony tv a bunch of us chipped in to get him for his birthday, to when he broke both his wrists at the same time (bad idea when you are a photographer), to the "Craw" story.
Dave and I had either picked up our friend Mary Pat (she of the recent trip to Hawaii fame) at the University of Illinois Circle campus in Chicago, or we were driving her there. It was a 6 hour drive. Through the better part of the drive, Dave kept urging Mary to say, "Go to sleep little craw." She refused time and time again. Finally after about 5 hours of pressure, she caved and said, "Go to sleep little, craw." With that, Dave curled up the fingers on his right hand and turned to the back seat, waving his hand and shouting, "Da Craw never sleeps!"
That was and that is Dave. His essence has not changed in all these years.
Tuesday, April 27, 2010
Group Health update
I also should bring you up to date on my continuing dialogue with Group Health regarding my lack of a treating oncologist.
When I returned from my visit to Kentucky yesterday, I emailed Dr. G at Group Health:
I then received this response from him today:
I guess what has really surprised and depressed me during all of this, is that no one at Group Health appears willing to make the tough decision. Which really isn't all that tough, if you think about it. All it consists of is saying, "No." I talked about it today with a fellow attorney who has had a few intense medical experiences with Group Health of her own, and is one of the best attorneys in my practice at understanding medical records and deposing medical witnesses. Her take on this is that doctors are conflict avoiders--they just don't like to say "no." That seems true to me, as I contrast my career as an attorney who engages in conflict with that of the doctors I not only know but have been related to--from great grandfathers, to grandfather, to great uncles, to father, brother, and now daughter. But it's better for me (and probably for more than just me) to have certainty, even if it is not the response I would like. Because then I can move on. Until I get that firm response, there is still an open question. And a lot of mush to drag along.
Sobeit.
When I returned from my visit to Kentucky yesterday, I emailed Dr. G at Group Health:
Dear Dr. G***,
Wow. It has been 18 full days since your first response to me but nothing since. I cannot tell you how very disappointed I am in this. Perhaps you could please do so?
Regina
I then received this response from him today:
Hi Regina,My response to Dr. G:
I have forwarded your message to the doctors in Oncology and they are ready to help you with your care. Do you have an appointment with any of the doctors in oncology? Dr. C** said they would be glad to see you and work with you on what was needed.
J
Dear Dr. G***,
As I put in my first email to you, I was asking for an answer to the question of whether I could get a referral to a lung cancer specialist. So I must interpret from this email GH's response is "No, GH will not refer me to a lung cancer specialist."
Why is it that no one at GH would say "no" to my original question? Instead, I was directed to 4 separate entities and finally I stopped the merry go round and addresse[d] it to you. And yet no one has yet said the word "no." You might want to consider why this is.
What it has meant is almost a month's delay in obtaining a treating oncologist. What I've been offered, via a form letter, is a referral to a doctor who is currently based in Tacoma, but who will be moving up to Group Helath [sic] when you find a replacement for her in Tacoma. I have absolutely no idea of what her curriculum vitae looks like, and whether she has treated lung cancer patients and is familiar with the treatment modalities and clinical trials particular to NSCLC. The form letter was generally designed for all cancer patients. Cancer is the one medical condition where one size really does not fit all. But that is the way that Group Health organizes and manages itself to deliver medicine. Which in most instances achieves favorable results. However, not in cancer. I have a dear friend who is also a cancer patient at GH and I've shared some of my experiences and stories with him about my treatment at GH and he was not surprised. Because he has his own.
I have an appointment with Dr. C******* tomorrow at 4pm to review my ct scans which will be taken earlier that day. Then we will move on from there.
Thank you.
Regina
I guess what has really surprised and depressed me during all of this, is that no one at Group Health appears willing to make the tough decision. Which really isn't all that tough, if you think about it. All it consists of is saying, "No." I talked about it today with a fellow attorney who has had a few intense medical experiences with Group Health of her own, and is one of the best attorneys in my practice at understanding medical records and deposing medical witnesses. Her take on this is that doctors are conflict avoiders--they just don't like to say "no." That seems true to me, as I contrast my career as an attorney who engages in conflict with that of the doctors I not only know but have been related to--from great grandfathers, to grandfather, to great uncles, to father, brother, and now daughter. But it's better for me (and probably for more than just me) to have certainty, even if it is not the response I would like. Because then I can move on. Until I get that firm response, there is still an open question. And a lot of mush to drag along.
Sobeit.
CT scan anxieties
My 4th ct scan ever is scheduled for tomorrow. It has been set for a month now.
The tension is just starting to hit tonight as I reflect on the possible outcomes. I already have detected a swollen lymph node in the subclavicular region of my neck on the left side. Therefore, I know it is not going to be a cake walk. There will be some negative news forthcoming, but I can't tolerate contemplating that the Tarceva is not working at all, particularly as my left leg looks like I walked through a fire ants' nest with shorts on. It's great for grossing out your mom when you are back visiting her in Lexington, KY, but not for those wee hours of the morning when you can't get to sleep because it is itching or throbbing.
And I learned that the ex spousal unit is remarrying. The happy day is set for August 8, at a lovely outdoor location in Seattle. It sets the stage for him to run for governor in 2012, if all the entrails are positively read and all the other omens fall in line. Of course, he didn't tell me. Just as he's never called to express concern as I deal with cancer. One of those things. We are both far different people than we were when we married 30 years ago, and when we divorced 11 years ago. However, our children are wonderful gifts regardless, and I am remain grateful for their existence and presence in my life.
So that's the short skinny of my anxieties.
On the plus side, our DeFeet Lung Cancer team remains the 3d highest fund raiser for the Lung Association of Washington. Go team! And thank you so much to everyone who contributed. This will be fun on Sunday. Even if it does rain. More on that later. And more to post tomorrow on the ct scans, good news or bad.
The tension is just starting to hit tonight as I reflect on the possible outcomes. I already have detected a swollen lymph node in the subclavicular region of my neck on the left side. Therefore, I know it is not going to be a cake walk. There will be some negative news forthcoming, but I can't tolerate contemplating that the Tarceva is not working at all, particularly as my left leg looks like I walked through a fire ants' nest with shorts on. It's great for grossing out your mom when you are back visiting her in Lexington, KY, but not for those wee hours of the morning when you can't get to sleep because it is itching or throbbing.
And I learned that the ex spousal unit is remarrying. The happy day is set for August 8, at a lovely outdoor location in Seattle. It sets the stage for him to run for governor in 2012, if all the entrails are positively read and all the other omens fall in line. Of course, he didn't tell me. Just as he's never called to express concern as I deal with cancer. One of those things. We are both far different people than we were when we married 30 years ago, and when we divorced 11 years ago. However, our children are wonderful gifts regardless, and I am remain grateful for their existence and presence in my life.
So that's the short skinny of my anxieties.
On the plus side, our DeFeet Lung Cancer team remains the 3d highest fund raiser for the Lung Association of Washington. Go team! And thank you so much to everyone who contributed. This will be fun on Sunday. Even if it does rain. More on that later. And more to post tomorrow on the ct scans, good news or bad.
Monday, April 19, 2010
DeFeet Lung Cancer
Oh I know. That's lame. But it's the name of the team I formed for the Lung Walk. So any and all who want to walk with me around the beautiful University of Washington campus Sunday May 2, should join up. Click the title of this post and you will be taken to the team website.
The event kicks off at 9:30am in Red Square, so I am thinking we should be there a bit before--say 9am or so. If you sign up, you even get a tshirt for a modest donation. I've set a goal of $500 in fundraising and 10 team members (but if my dear generous readers meet this goal, I may set it higher). Many thanks to friends Katy, Ann, Olive and Janet who have already contributed to the cause and will be there in spirit. And intrepid team members Susan, Diane, and Andrea. You RAWK!
Update: we're no. 3 in terms of money raised last week. Cool beans guys!
The event kicks off at 9:30am in Red Square, so I am thinking we should be there a bit before--say 9am or so. If you sign up, you even get a tshirt for a modest donation. I've set a goal of $500 in fundraising and 10 team members (but if my dear generous readers meet this goal, I may set it higher). Many thanks to friends Katy, Ann, Olive and Janet who have already contributed to the cause and will be there in spirit. And intrepid team members Susan, Diane, and Andrea. You RAWK!
Update: we're no. 3 in terms of money raised last week. Cool beans guys!
Sunday, April 18, 2010
Yet ANOTHER Group Health story
I've been waiting for a while, hoping that this would resolve itself and I could forget about it, but it has not. I've been on a slow boil for a while over it and tonight the pot just blew up for me.
I've been without an oncologist for about three weeks now.
That's right, I do not have a specialist who is assigned to assist me in my treatment for cancer at Group Health. My former oncologist left GH abruptly at the end of March. At the time of his departure, I spoke with a friend of mine, L, who is a gynecological surgeon at Virginia Mason. She suggested because of the relationship between Group Health and Virginia Mason, that I ask to be referred to a VM oncologist for treatment. She recommended Dr. O. So I took her recommendation to heart and emailed the head of oncology at GH. He was on vacation and I received an 'out of office' response directing any questions in his absence to Dr. F. So I forwarded my email to Dr. F. He wrote me back and said that Dr. O at VM was an esophageal oncologist, not a lung cancer specialist, and thus I could not be referred to him. Fair enough.
I waited several days for the head of oncology to return and then emailed him, mentioning my correspondence with Dr. F, and requesting a referral to Dr. M at Seattle Cancer Care Alliance because he WAS a lung cancer specialist. Head of oncology responded that in order to get a referral, I had to get the approval of the business office. Ok.
Next day I called the business office of Group Health and was told that I needed the referral to come from my attending physician. Ok.
I emailed my primary care physician, requesting the referral, and received a response that I needed to get oncology to make the referral.
Once again, I emailed the head of oncology requesting the referral. Head of oncology emailed back that I needed to get the referral from the business office.
Does anyone see a problem here?
So. I decided to email Dr. G, VP for Group Health. Here is the text of my email to him:
That email was sent April 7. The next morning, I received the following from Dr. G:
That was hopeful, I thought.
So I waited. And waited. And waited. Finally on April 14, I sent the following to Dr. G:
I have heard nothing from Dr. G.
However, on April 14, I did receive in the mail a form letter, probably addressed to all of Dr. N's former patients that informed me that I needed to get a treating oncologist and that all the Seattle oncologists were pretty booked up with patients. Therefore Dr. C, the head of oncology, was recommending that I sign up with a Dr. G, who is a great oncologist, except she is based in Tacoma, although she was moving to Seattle sometime--as soon as they found a replacement for her in Tacoma.
I just feel so special.
I've been without an oncologist for about three weeks now.
That's right, I do not have a specialist who is assigned to assist me in my treatment for cancer at Group Health. My former oncologist left GH abruptly at the end of March. At the time of his departure, I spoke with a friend of mine, L, who is a gynecological surgeon at Virginia Mason. She suggested because of the relationship between Group Health and Virginia Mason, that I ask to be referred to a VM oncologist for treatment. She recommended Dr. O. So I took her recommendation to heart and emailed the head of oncology at GH. He was on vacation and I received an 'out of office' response directing any questions in his absence to Dr. F. So I forwarded my email to Dr. F. He wrote me back and said that Dr. O at VM was an esophageal oncologist, not a lung cancer specialist, and thus I could not be referred to him. Fair enough.
I waited several days for the head of oncology to return and then emailed him, mentioning my correspondence with Dr. F, and requesting a referral to Dr. M at Seattle Cancer Care Alliance because he WAS a lung cancer specialist. Head of oncology responded that in order to get a referral, I had to get the approval of the business office. Ok.
Next day I called the business office of Group Health and was told that I needed the referral to come from my attending physician. Ok.
I emailed my primary care physician, requesting the referral, and received a response that I needed to get oncology to make the referral.
Once again, I emailed the head of oncology requesting the referral. Head of oncology emailed back that I needed to get the referral from the business office.
Does anyone see a problem here?
So. I decided to email Dr. G, VP for Group Health. Here is the text of my email to him:
Dear Dr. G,
I am writing to you because I don't know where to turn at this point.
As you may recall, I am a friend and former patient of C. She sent me to you late last year when issues with my lung cancer care at Group Health came up, and you were of great assistance to me at the time.
I now have another issue and am turning once again to you for help.
My treating oncologist, Dr. N, has left Group Health. I was only recently made aware of his permanent departure. L M, a friend and a gynecological surgeon at Virginia Mason suggested that I request Virginia Mason oncologist, Dr. O, be put in charge of my care. I raised this issue with Dr. F last week in an email, because Dr. C was out of the office, and Dr. F responded that Dr. O was not a lung cancer specialist but rather dealt with esophageal cancers. So I wrote to Dr. C and asked if I could be referred to Dr. RM at Seattle Cancer Care Alliance, as he was a lung cancer specialist. Dr. C responded that this was an issue I would have to take up with GH's business office. So I called Group Health's business office and was told that a referral had to come from my GP. So I emailed Dr. Mc and requested that a referral to Dr. M be made, and I was told that I had to get such a referral from the oncology department. So again, I wrote to Dr. C and requested a referral. I then received an email from Dr. C that I had to get approval from the business office.
So we have come full circle. And I am no closer to knowing whether I can have my case referred to Dr. M or not. Frankly, I am feeling abandoned by the health care folks at Group Health, yet again. If I have gone to every single place I have been referred to and no one has given me an answer. If the answer is no, then just say so. But it seems to me that if a referral were made by oncology, that would suffice for the business office when the bills came in. At least that's how it works at Regence, where I have a friend who works in the administration there.
I am currently not under the care of any oncologist and I would like for that state of limbo to end. Dr. C seems to think that the oncology department at Group Health is sufficient to treat my lung cancer, but I have some issues with that. For example, there has been no genetic testing of my tumors as Dr. M recommended when I had my second opinion consult with him in October, 2009. And last week I read in Cure magazine that genetic testing should be employed right off the bat, when devising treatment for lung cancer. I am currently on Tarceva as a second line treatment since the first line chemotherapy was revealed to have failed in a December ct scan. The Tarceva was shrinking or holding the tumors' sizes steady per the ct scan in Feb. But my prescription of Tarceva was sort of dumb luck in that there had been no testing of the tumors for the EGFR mutation. I would think that an oncologist familiar with lung cancer and the most recent protocols for treatment would know how critical genetic testing was to successful treatment, and would have suggested this at the outset of my treatment.
So, Dr. G, who at Group Health should I direct my questions to concerning a referral to Dr. M for treatment of my lung cancer?
Thank you.
Sincerely,
Regina Cullen
That email was sent April 7. The next morning, I received the following from Dr. G:
Dear Regina,
Thank you for taking the time to write. First, please know I am sending you gentle thoughts as you struggle with your cancer. I am sorry that you are feeling abandoned and will work on trying to resolve this for you today.
JG
That was hopeful, I thought.
So I waited. And waited. And waited. Finally on April 14, I sent the following to Dr. G:
Dear Dr. G,
I realize that these things can take time, but time is relative, particularly when one is suffering from stage III/IV lung cancer. You did mention last Thursday that you were trying to resolve it that day.
I look forward to hearing from you.
Regina
I have heard nothing from Dr. G.
However, on April 14, I did receive in the mail a form letter, probably addressed to all of Dr. N's former patients that informed me that I needed to get a treating oncologist and that all the Seattle oncologists were pretty booked up with patients. Therefore Dr. C, the head of oncology, was recommending that I sign up with a Dr. G, who is a great oncologist, except she is based in Tacoma, although she was moving to Seattle sometime--as soon as they found a replacement for her in Tacoma.
I just feel so special.
Tuesday, April 13, 2010
Snake Oil Salesmen R Us
.jpg)
Since my diagnosis of lung cancer back in September, I've come to see my life journey take a few unplanned and unexpected detours. It's a multi layered, shorter version of what I had envisioned, but it's rather more in focus these days because, well, mortality does that to you.
Some of the unexpected detours I've taken, have been to various cancer sites on the internet. There are blogs such as mine, that I visit and try keep up with the authors, such as my friend and former college classmate, Louisa, who is struggling with stage IV ovarian cancer. Then there are the sites formed to be a community for those suffering from the same sorts of cancer. There's the Inspire site, and there's the LungLove site, and there's probably more out there that I have not found yet. I've been going to the Inspire site for about two months now. And there's a lot of pain and death on there. Lung cancer is not gentle and it is not lazy. It kills rapidly, particularly as symptoms don't manifest until the disease is in its last stages. And successful scientific treatment modalities are rare or in their infant stages.
As a result, there are many very fearful, desperate people out there, whether they are the patients or their loved ones who are their caregivers. And, desperate, fearful people are a class of folks that are easily victimized. We see this throughout American history. And we've named such medical quacks Snake Oil Salesmen. Earlier in my life, I thought that perhaps most snake oil salesmen went out of business with the death of patent medicines such as Serutan ("that's 'nature' spelled backwards). I think it was the sponsor of the Amateur Hour on early television. But what I've found, particularly on the chat board at inspire.com is that these snake oil salesman have transformed themselves from the stereotype pictured above and sound just as educated as medical doctors. In fact, some of them are medical doctors. But what this group of hucksters has for customers today are not the bumbling small town yokels of yore, but folks like those I've met on the cancer community websites who are not being helped by FDA approved chemotherapy or other cancer treatments. This is a remarkably potent audience for modern snake oil salesmen, one that will pay whatever it takes, if they can just be convinced that the coffee enemas, the electronic zappers, the colon cleanses, or the shark cartilage injections have cured someone else's cancer, and thus are likely to help cure them.
How is it that we, some of the best educated people in the world, can fall prey to sharpsters like these? I think it's a combination of desperation when conventional treatments don't work, combined with a failure to understand modern day science. Gene splicing techniques and much of the logic behind gene therapy is not easy to comprehend for most people. Furthermore, understanding statistics remains more like reading Greek, even to those journalists paid to report on it--witness the confusion over the results of some study about the effect of birth control pills on breast cancer rates actually mean. I remember reading hysterical accounts in the press about this several years ago, and then my OB/GYN telling me that the actual increase in cancer rates from taking birth control pills was minuscule at best. Is it any wonder then that so many in the US become disillusioned with modern medicine?
My feelings on this subject came to a head tonight when I watched New Yorker science writer Michael Specter on Ted.com. I recommend that you click on the link and view it for yourself. The one point from this video that I took away, and it should be emphasized again and again, is that you can have your own opinion, but you are not entitled to your own facts. My own favorite admonition along these lines, as my loyal readers will recall, is: the plural of anecdote is not data.
This disregard and dismissal of modern day science must stop, else we return the human race to the nasty, brutish and short existence that predated the introduction of vaccines.
I am not very good at pointing others' defects in reasoning out to them without sounding snide or superior. Rather like Michael Specter. I am still working on a way to try to enter into a convincing dialogue with some of those members on Inspire, for example, who think that the American Cancer Society is in the back pocket of the pharmacy industry, and who are busy recommending to other members that they try the latest naturopathic remedies. Some are even touting laetrile these days! I just haven't figured out how to break through their fears to reach them.
Monday, April 12, 2010
What are you doing May 2d?

I'll be doing something a bit new to me. I'll be participating in the Lung Walk, sponsored by the American Lung Association. My friend Andrea mentioned it to me, so I signed up tonight. Although the American Lung Association spreads itself pretty thin covering all the possible things that can go wrong with lungs, it still does some very good work in the area of lung cancer.
Do you want to walk with me? If I get enough folks who don't mind spending a Sunday morning walking around the University of Washington campus with me, we could have a team. And make up a cool team name like Moe's Misbegotten. Or, if you can't make it because of distance, you could consider donating a few bucks. I'm not really a very good fundraiser, am I? I'll work on that in the coming months.
Here's the website to sign up. It would be wonderful to see you all. And we get tshirts!! That means I can replace the one I had made almost 30 years ago that reads: "Dog being walked against Reagan." Some things never change, do they?
Scooter update and Truffle too!

I picked Scooter up Saturday morning and he was very glad to see me. But he was definitely recuperating, moving a bit more gingerly than is his normal pattern. Usually when I slide open the door from the kitchen to my deck he is barking furiously and springs off the deck to the ground below, all the better to catch the squirrels that he is sure are lurking around the bird feeders in the back. Well, he's taking the stairs these days and not barking quite so much.
But not to be outdone, Truffle has ringworm! Ringworm, I learned, is not a parasite but a fungal infection. So, I took Truffle to NE Veterinary this am and the vet pulled some hair in the discolored circle about the size of a quarter that has formed on her back. The ringworm will not be fully confirmed until the testing is complete, but in the interim, I am to give her topical antibiotics on the infected site twice a day. That's easy. I just give Scooter his oral antibiotics then too. Add in my athlete's foot meds and we're all just one happy family here.
Good thing Max seems to be doing fine (knock on wood).
Happy Monday to everyone.
Thursday, April 08, 2010
Scooter visits the surgeon

Up this morning and into the kitchen. Discovered that I had not let Scooter, my 7 year old dachshund, out in time. I could tell the puddle was his because it was not a lake, which it would have been had it been Max the labrador with the super size kidneys, and it was red. Scooter was treated for a urinary tract infection back in January and I had never followed up on it because it is difficult to get a urine sample from a dog who is so close to the ground and who refuses to pee when on a walk (really). Sensing opportunity was at hand, I grabbed the turkey baster from my utensil drawer and managed to obtain a sample large enough to take into the vet's this afternoon.
Scooter definitely had blood and sedimentation present in his urine and I agreed to an xray which showed a rather large stone in his bladder. Have to confess that while he was out getting his xray, I got rather teary eyed. It came a bit too close to my situation for comfort. My sister, the vet, told me later that a bladder stone is far better for Scooter than a kidney stone, which would be much more involved surgery. As it is, the final price tag for the excision is upwards of $1000. Ah well. He is a good guy and definitely worth it. I think he'll feel much better afterwards.
Anyway, I deliver him tomorrow to NE Veterinary. Say a little doggy prayer for him, if you are so inclined. Thank you.
The consolidated read of my ct scans
I promised in my prior post to add in the radiologist's answers to the questions I posed concerning my 3 sets of ct scans that have been done of my neck and chest. Rather than add them to that post, I offer it here separately because the doctor mixed her responses in with my original email. The doctor's comments are italicized to dstinguish them from email as the paragraphs were somewhat rearranged from my original.
Mrs Cullen,
I have answered some of the questions that you have directed to Dr. N*****. I hope the answers help you somewhat.
I want to impress to you that the reports that we generate are to be read by physicians. The terms of anatomical descriptions and jargon that we use are standard with some variations. All the reports I reviewed are using variations that are within the accepted norm. Often, we edit or omit to report findings that may not be significant when we report. For example, a patient has 20 lung nodules we (at least I) may not describe them all because there is no difference between having 10 lung nodules versus 20.
M****** O*, MD
Central radiology
Additional questions:
1. Why are there 6 identified node sites with cancer in the 12/09/09 lung ct scan and only 5 in the other two lung ct scans?
Sometimes we miss reporting a node/nodule/mass. The nodule that you refer to was there but was not reported on the initial study. Unfortunately, on these lung nodules, it is quite difficult. We do our best but sometimes, they get missed. For lungs, we review apporoximately 90 to 100 images. Due to technical factors, small nodules can be easily overlooked because they look very much like normal vessels in the lungs. We look at images back and forth multiple times but we do miss them from time to time.
Even if we find them, there is another issue of whether these are cancer or not. No one knows for certain. We make inferences based on the total number, appearance, interval growth. This is why follow up scans are so important.
Perhaps, Dr N***** can point out the nodules versus adjacent vessels to you when you visit next.
2. Do you think that having different radiologists read the exams can create inconsistencies?
There is always inter-observer variability. However, we try to use similar language to describe what we see. Ultimately, it is the images themselves that give the final answer. We have to line up the CT images at the exact same location on the computer and measure the abnormality. Even if the wording may be selected differently, the important fact is if the nodules are getting either smaller or larger. This information is not confusing to the referring physicians. If there is a concern from the referring physicians point of view, we coordinate with that physician so that there is no misunderstanding.
Would it be too much to ask that one very good radiologist sit down with all three of my ct scans, and read them, to give a more uniform interpretation of the development/shrinkage of my tumors?
I think the information has been conveyed to the referring oncologist, Dr N*****, without confusion regarding what is happening in your case. Your masses/nodules are all shrinking. If the referring oncologists are confused regarding our reports, and wishes to have one radiologist read all of the studies, then we can pursue that. However, if the radiologist that reads your study is on vacation for 2 weeks, for example, then the study will not be read for that duration. There are other logistical issues regarding such specified arrangements. For example, I only work 3 days or so every week (as do many other radiologists who work part time), and the CT would sit waiting until I returned to work 4 to 5 days later. Again, if you wish so, we can arrange for it.
3. What is going on with the neck scans? I really don’t know what the reading on the last one means.
Very evident left vocal cord paralysis today. Stable
adenopathy in the low left neck.
This is impression from your most recent neck CT. The impression from the reading radiologist is that the adenopathy is stable. Form that statement, I make an inference that there are no new findings. I do not understand your question.
B. Lung (reader: M****** O*, MD)
1. Paraspinous location of left lower lobe, 22 x 16 mm previously 30 x 22 mm at same location (there’s no nodule that matches this measurement in the 12/09/09 lung ct scan—which one is she talking about?)
As radiologists, we do not use other people’s reports as much as the images that are in front of us. The images “save” the measurements that the last radiologists have used. Unfortunately, the measurements from the study from 9/16/09 were not saved with the study, a computer glitch. Therefore, I had no record of what image was measured. Therefore, I needed to re-measure the nodules (mass is another word that we use to describe nodule). I could not get 2.6x2.1cm (which is what Dr Burns did). I reported what I measured and compared to what I got on the 2/19/10 study. What is important is that the size is decreasing, measured at the exact same location. I suppose that I probably did not have to give the re-measurement from Sept, which would not have lead to confusion. However, I wanted to emphasize that the mass is decreasing considerably so I gave the measurement that I made.
2. Right lower lobe posterior nodule, 4mm, down from 5mm (which one is she referring to here?)
This was reported in 12/9/09 but not in Sept 2009.
3. Left upper lobe anterior lesion appears slightly smaller and less plump as well (is this the apical nodule, B.4 from the 12/09/09 lung ct scan? If not, which is it?)
Apical = left upper lobe. Apical actually refers to very highest point of left upper lobe. Even in the same day and on the same scan, we may call it apical or left upper lobe, when describing the location. This is never confusing to the referring clinicians.
4. Subplueral posterior left lower lobe superior segment, 9mm-- previously 15 mm (which one is this?)
Yes. Again, these are descriptions that we use that we understand to be the same.
5. Adenopathy in the AP window decreased, 32 x 14 mm (is this B.1 in the 12/09/09 lung ct scan? If not, which is it?)
yes
AP window = aortopulmonary window = aortopulmonic window.
A. Neck (reader: A*** N**, MD)
1. right thyroid lobe, 5mm nodule –is this cancer?
2. left thyroid lobe, 2mm—is this cancer?
Thyroid nodules are very prevalent in normal population, as much as 70 to 80% of people. Only a tiny proportion of nodules are cancer. Unless there is a reason to pursue these nodules, we do not pursue them for the presence of cancer. There are criteria that determine if they need to be pursued. Since they are there, they were reported.
3. Pretracheal node, 13mm—is this cancer?
We use a size criteria to describe if something is abnormally enlarged or not. We have no idea of knowing if something is cancerous or not unless it is biopsied. We can give an educated guess regarding any node based on size, interval growth, and morphology. A 13mm node is abnormally enlarged node in this location. The abnormality is based on the statistical analysis of all nodes that are seen in the chest and the biopy correlations that were done as a clinical study performed many years ago. (We use the knowledge base that is generated over many years of clinical data accumulation.) It is up to the oncologist, surgeon, and the patient combined with the imaging information to decide if this is something that needs definitive answer or not, which will require biopsy. In your particular case, we know that you have metastastic lung cancer. Whether this particular node has cancer or not does not change your cancer staging. The staging information is what is used to direct therapy, not whether or not each nodule is cancerous. Dr N***** can probably explain this to you better.
4.Heterogenous mass seen in aortopulmonic window, 24 mm (what’s the difference between this and the aorticopulmonary window?)
They are both routinely accepted ways of describing the same thing.
Mrs Cullen,
I have answered some of the questions that you have directed to Dr. N*****. I hope the answers help you somewhat.
I want to impress to you that the reports that we generate are to be read by physicians. The terms of anatomical descriptions and jargon that we use are standard with some variations. All the reports I reviewed are using variations that are within the accepted norm. Often, we edit or omit to report findings that may not be significant when we report. For example, a patient has 20 lung nodules we (at least I) may not describe them all because there is no difference between having 10 lung nodules versus 20.
M****** O*, MD
Central radiology
Additional questions:
1. Why are there 6 identified node sites with cancer in the 12/09/09 lung ct scan and only 5 in the other two lung ct scans?
Sometimes we miss reporting a node/nodule/mass. The nodule that you refer to was there but was not reported on the initial study. Unfortunately, on these lung nodules, it is quite difficult. We do our best but sometimes, they get missed. For lungs, we review apporoximately 90 to 100 images. Due to technical factors, small nodules can be easily overlooked because they look very much like normal vessels in the lungs. We look at images back and forth multiple times but we do miss them from time to time.
Even if we find them, there is another issue of whether these are cancer or not. No one knows for certain. We make inferences based on the total number, appearance, interval growth. This is why follow up scans are so important.
Perhaps, Dr N***** can point out the nodules versus adjacent vessels to you when you visit next.
2. Do you think that having different radiologists read the exams can create inconsistencies?
There is always inter-observer variability. However, we try to use similar language to describe what we see. Ultimately, it is the images themselves that give the final answer. We have to line up the CT images at the exact same location on the computer and measure the abnormality. Even if the wording may be selected differently, the important fact is if the nodules are getting either smaller or larger. This information is not confusing to the referring physicians. If there is a concern from the referring physicians point of view, we coordinate with that physician so that there is no misunderstanding.
Would it be too much to ask that one very good radiologist sit down with all three of my ct scans, and read them, to give a more uniform interpretation of the development/shrinkage of my tumors?
I think the information has been conveyed to the referring oncologist, Dr N*****, without confusion regarding what is happening in your case. Your masses/nodules are all shrinking. If the referring oncologists are confused regarding our reports, and wishes to have one radiologist read all of the studies, then we can pursue that. However, if the radiologist that reads your study is on vacation for 2 weeks, for example, then the study will not be read for that duration. There are other logistical issues regarding such specified arrangements. For example, I only work 3 days or so every week (as do many other radiologists who work part time), and the CT would sit waiting until I returned to work 4 to 5 days later. Again, if you wish so, we can arrange for it.
3. What is going on with the neck scans? I really don’t know what the reading on the last one means.
Very evident left vocal cord paralysis today. Stable
adenopathy in the low left neck.
This is impression from your most recent neck CT. The impression from the reading radiologist is that the adenopathy is stable. Form that statement, I make an inference that there are no new findings. I do not understand your question.
B. Lung (reader: M****** O*, MD)
1. Paraspinous location of left lower lobe, 22 x 16 mm previously 30 x 22 mm at same location (there’s no nodule that matches this measurement in the 12/09/09 lung ct scan—which one is she talking about?)
As radiologists, we do not use other people’s reports as much as the images that are in front of us. The images “save” the measurements that the last radiologists have used. Unfortunately, the measurements from the study from 9/16/09 were not saved with the study, a computer glitch. Therefore, I had no record of what image was measured. Therefore, I needed to re-measure the nodules (mass is another word that we use to describe nodule). I could not get 2.6x2.1cm (which is what Dr Burns did). I reported what I measured and compared to what I got on the 2/19/10 study. What is important is that the size is decreasing, measured at the exact same location. I suppose that I probably did not have to give the re-measurement from Sept, which would not have lead to confusion. However, I wanted to emphasize that the mass is decreasing considerably so I gave the measurement that I made.
2. Right lower lobe posterior nodule, 4mm, down from 5mm (which one is she referring to here?)
This was reported in 12/9/09 but not in Sept 2009.
3. Left upper lobe anterior lesion appears slightly smaller and less plump as well (is this the apical nodule, B.4 from the 12/09/09 lung ct scan? If not, which is it?)
Apical = left upper lobe. Apical actually refers to very highest point of left upper lobe. Even in the same day and on the same scan, we may call it apical or left upper lobe, when describing the location. This is never confusing to the referring clinicians.
4. Subplueral posterior left lower lobe superior segment, 9mm-- previously 15 mm (which one is this?)
Yes. Again, these are descriptions that we use that we understand to be the same.
5. Adenopathy in the AP window decreased, 32 x 14 mm (is this B.1 in the 12/09/09 lung ct scan? If not, which is it?)
yes
AP window = aortopulmonary window = aortopulmonic window.
A. Neck (reader: A*** N**, MD)
1. right thyroid lobe, 5mm nodule –is this cancer?
2. left thyroid lobe, 2mm—is this cancer?
Thyroid nodules are very prevalent in normal population, as much as 70 to 80% of people. Only a tiny proportion of nodules are cancer. Unless there is a reason to pursue these nodules, we do not pursue them for the presence of cancer. There are criteria that determine if they need to be pursued. Since they are there, they were reported.
3. Pretracheal node, 13mm—is this cancer?
We use a size criteria to describe if something is abnormally enlarged or not. We have no idea of knowing if something is cancerous or not unless it is biopsied. We can give an educated guess regarding any node based on size, interval growth, and morphology. A 13mm node is abnormally enlarged node in this location. The abnormality is based on the statistical analysis of all nodes that are seen in the chest and the biopy correlations that were done as a clinical study performed many years ago. (We use the knowledge base that is generated over many years of clinical data accumulation.) It is up to the oncologist, surgeon, and the patient combined with the imaging information to decide if this is something that needs definitive answer or not, which will require biopsy. In your particular case, we know that you have metastastic lung cancer. Whether this particular node has cancer or not does not change your cancer staging. The staging information is what is used to direct therapy, not whether or not each nodule is cancerous. Dr N***** can probably explain this to you better.
4.Heterogenous mass seen in aortopulmonic window, 24 mm (what’s the difference between this and the aorticopulmonary window?)
They are both routinely accepted ways of describing the same thing.
Tuesday, April 06, 2010
Waiting for the Electrician or Someone Like Him
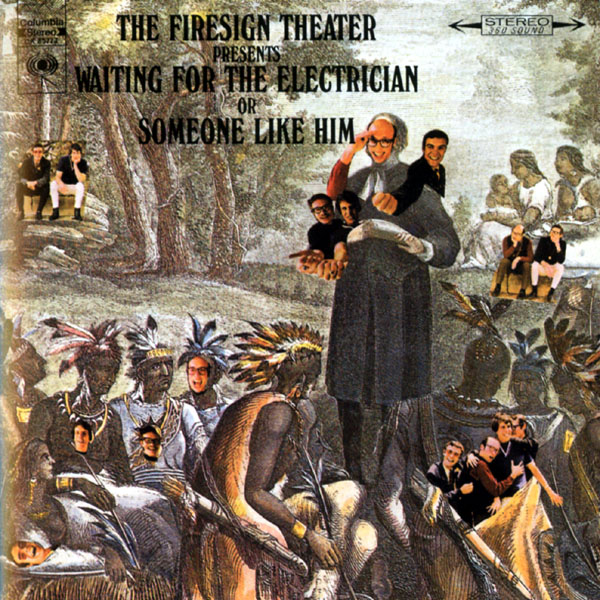
I'm betraying my hippie roots tonight, but there is a point, although it will probably take too long to get to it for most of you who didn't stay up way too late to listen to these guys in your misspent youth.
Ah well. On to the past...
I had an ultrasound of my upper right chest and shoulder and right arm Monday afternoon. No blood clots were found, for which I am grateful. I have changed my sleeping arrangements, which is relatively easy to do when your bed companions are two miniature dachshunds, so that now I am perched on the side of the bed (those dachshunds may be small but they like to crowd right up next to you) where it's easiest to sleep on my left side. This seems to have alleviated the pain symptoms on my upper right side from last week. I am hopeful that this is auspicious news for my port.
I went to Group Health this afternoon to pick up my new glasses. My current pair is 4 years old and while fairly serviceable, the lenses are scratched and in need of polishing. Or so I thought. When I picked up my new glasses, I mentioned to the optician that I wanted to leave my old glasses so the lenses could be polished. "You could do that," he responded, "but we use a very caustic agent to strip the lenses and they could end up all white." And why would that be? I inquired. He explained that the anti reflective coating on my glasses was responsible for my inability to clean the scuffing off the lenses by myself, and that's why it would have to be done in a chemical vat--to remove the coating. With not a very good chance that the lenses would actually be clean in the end. Ah. Right. That would be the same reflective coating that I agreed to apply to my new lenses when I purchased them last week for an additional $70 and nothing was disclosed to me at that time about this, right? Right. Figures.
This evening I went to a panel discussion at the University of Washington in Kane Hall. The topic was: New Discoveries in Medicine: Implications for the Cost and Quality of American Healthcare Panel Discussion. On the panel were 4 eminent physicians: a doctor from Group Health, one from Harvard Medical School, a doctor from Amgen and the dean of the UW medical school. The discussion was very interesting, even if they did not answer the two questions I wrote down and submitted to the group. But one of the topics that was touched on as sort of a pathway for the future was standardization of protocols. It was mentioned in connection with treatment of low back pain, which is of interest to me professionally as I do worker's compensation cases for a living and low back pain is a major cause of the cases that are heard by the Board of Industrial Insurance Appeals. Standardizing care for low back pain would definitely make my work, and the work of the Board easier. However, I'll believe it when I see it.
My scepticism is further reinforced by my own experience with respect to the multiple doctors who have read ct scans that I have had since I was diagnosed with lung cancer. I have had ct scans on Sept. 16, 2009, December 9, 2009, and February 19, 2010. Each time scans were taken of the neck and of the chest. Each time one doctor read the neck scan and one doctor the chest scan. Of the six scans, there were five different doctors doing the reads. Is it any wonder that if you took all six of those scans and read them together you might be a bit confused? Just so you can get a better idea of the confusion, I am posting the letter I sent to my oncologist on February 20, 2010, outlining my problems in understanding:
Dear Dr. N***,
Tonight I reviewed all of the ct scans done on my neck and lungs--that would be 3 for each--and I have a number of questions based upon them. To begin with, I summarized each of the ct scans and then after each nodule, the radiologist identified as cancerous, I put my question in parenthesis. There are additional questions at the end as well. I hope we can discuss these at some length next week.
September 16, 2009, CT scan:
A. Neck (reader: Dr A**** N**, MD)
1. right thyroid lobe, 5mm nodule (is this cancer?)
2. left thyroid lobe, 2mm (is this cancer?)
3. Pretracheal node, 13mm (is this cancer?)
4.Heterogenous mass seen in aortopulmonic window, 24 mm (what’s the difference between this and the aorticopulmonary window?)
B. Lung (reader: J*** B***, DO)
1. Left lower lobe lung mass, 2.6 x 2.1 cm
2. Smaller left lower lobe posterior subpulmonary nodule,1.3 x 1.0 cm
3. Left upper lobe pulmonary nodule, 4mm
4. Aorticopulmonary window, 2.3 x 1.4 cm
5. Precarinal lymph node, 1.2 x .8cm
December 9, 2009, CT scan:
A. Neck (reader: A**** N**, MD)
1. Interval enlargement of a lymph node; currently 11mm, as compared to 7 mm previously (where? I don’t find this on the 9/16/09 neck ct scan)
2. Anterior supraclavicular region node, 13mm—previously measured at 11.3mm (again, where is this found on the 9/16/09 ct scan?)
B. Lung (reader: J******** K****, MD)
1. AP window, centrally necrotic mass, 1.8 cm unchanged (really? It shows as 2.3 x 1.4 according to the ct scan above)
2. Dominant mass inferior medial left lower lobe decreased in size to 2.3 x 1.8 x 1.7 cm—previously 2.8 x 2.2 x 2.2 cm (Is this no. 1 in the 9/16/09 lung ct scan above? Numbers don’t match)
3. More cranial left lower lobe mass unchanged, 1.1 cm (which one is this? I don’t see it above)
4. Left apical noncalcified nodule unchanged, 4 mm (is this no. 3 from the 9/16/09 ct scan above?)
5. Noncalcified nodule in left lung base unchanged, 5 x 2mm (where is this on the 9/16/09 ct scan?)
6. Densely calcified granuloma in right lower lobe, 4mm (is in the right lobe of the lung as opposed to the left lobe and is this cancer?)
February 19, 2010 CT scan:
A. Neck (reader: C********* K*******, MD)
1. 3 nodes in a vertical row anterior to scalene musculature, overall size unchanged compared to 12/09/09 ct scan (12/09/09 scan describes only 2 nodes—so what gives here? And is this a problem that they are not shrinking?)
B. Lung (reader: M******** O*, MD)
1. Paraspinous location of left lower lobe, 22 x 16 mm previously 30 x 22 mm at same location (there’s no nodule that matches this measurement in the 12/09/09 lung ct scan—which one is she talking about?)
2. Right lower lobe posterior nodule, 4mm, down from 5mm (which one is she referring to here?)
3. Left upper lobe anterior lesion appears slightly smaller and less plump as well (is this the apical nodule, B.4 from the 12/09/09 lung ct scan? If not, which is it?)
4. Subplueral posterior left lower lobe superior segment, 9mm-- previously 15 mm (which one is this?)
5. Adenopathy in the AP window decreased, 32 x 14 mm (is this B.1 in the 12/09/09 lung ct scan? If not, which is it?)
Additional questions:
1. Why are there 6 identified node sites with cancer in the 12/09/09 lung ct scan and only 5 in the other two lung ct scans?
2. Do you think that having different radiologists read the exams can create inconsistencies? Would it be too much to ask that one very good radiologist sit down with all three of my ct scans, and read them, to give a more uniform interpretation of the development/shrinkage of my tumors?
3. What is going on with the neck scans? I really don’t know what the reading on the last one means.
I sent this to my oncologist and he had one of the radiologists read the scans and although I would love to post the consolidated report, the Group Health site is down tonight, so that will have to wait for tomorrow. However, to tie this back into the panel discussion on standardization from tonight, it was suggested that rather than just one doctor doing the reading for these six ct scans, it would be far better to put all five of the radiologists together and they could jointly come up with the correct reading. Rather like what a jury does with a civil or criminal trial. I like it. Sounds good to me. Except for the price tag. Which is always the 800 lb purple cow in the middle of the room.
So I guess I will continue to wait for the electrician. Or someone like him.
Saturday, April 03, 2010
Any port in the storm

Since Tuesday, I've been having a generalized,dull ache in my right upper chest and Friday night, I discovered that I could not leave my right hand in any sort of resting position for long without pain. Moving or stretching it would give me about 30 seconds of relief. I think it has to do with my port, which is inserted on the upper right side of my chest. At least I hope so, because all the cancer tumors so far discovered have been on the left side. I really don't want it to be spreading to my right side. No fever, no swelling around the port site, just a dull ache that would sometimes radiate down my right arm as well. So, I called the Urgent Care nurse at Group Health around 10 pm and she directed me to come into the Capitol Hill Urgent Care Center, which I did with my very kind friend Anne.
Despite my own diagnosis that these symptoms had to do with my port, the doc on call did another set of xrays--frontal view and left(!)side--and another panel of blood work, neither of which showed anything. The nurse who drew the blood from my port was not very adept in the procedure, which you can see in the above illustration, and the draw was excruciatingly painful with my port site remaining tender for the half hour the needle stayed inserted. This had never happened before in my experience.
However, once the doc determined that no more blood was required and no injections were needed, the port was flushed with heparin to take care of any possible clots that might have formed in the general vicinity, and the needle removed. I returned Anne to her house, got home at 2am, and let the dogs out. However, it did not keep Max from getting me up for yet another trip to the back yard at 4:50 am.
Saturday, the ache was not quite as overwhelming, but it remains in the background. More and better distractions, please! Too bad I have run out of Doc Martin tv episodes to watch(here's a question for you: would you rather be treated by Dr. Gregory House or Dr. Martin Ellingham?). I still have no explanation for the cause of my continuing chest discomfort. It would help if I had an oncologist. Monday...
And for those of my readers who celebrate, Happy Easter! As many of you know, I am, at best, a rather irreverent Presbyterian. Found this description of the Christian celebration that is worth sharing:
Easter is when Jesus came out of his cave, saw his shadow and said there were only six more weeks until Armageddon!
Or as Sandra Boynton put in one of her Easter cards: "How do you say Easter is a good idea in French? -open the card- C'est une Bonne idee." With a large Boynton picture of a rabbit under it. Meaning it's a Bunny Day.
I love Sandra Boynton.

Subscribe to:
Comments (Atom)





